|
|
|
|
What
are antibiotics?
Antibiotics are among the most powerful and important medicines
known. When used properly they can save lives, but used improperly,
they can actually harm your child. Antibiotics should not be used
to treat viral infections. Bacteria
and viruses
Two main types of germs- bacteria and viruses- causes most infections.
In fact, viruses cause most coughs and sore throats and all colds.
Bacterial infections can be cured antibiotics, but common viral
infections never are. Your child recovers from these common viral
infections when the illness has run its course. Make a habit of
asking your doctor why your child is given antibiotics?
Resistant
bacteria
New strains of bacteria have become resistant to antibiotics.
These bacteria are not killed by the antibiotic. Some of these
resistant bacteria can be treated with more potent antibiotics
which may need to be given by vein (IV) in the hospital, and a
few are already untreatable. The more antibiotics prescribed,
the higher the chance that your child will be infected with resistant
bacteria.
How
bacteria become resistant?
Each time we take antibiotics, sensitive bacteria are killed,
but resistant ones may left to grow and multiply. Repeated use
and improper use of antibiotics are some of the main causes of
the increase in resistant bacteria. These resistant bacteria can
also be spread to others in the family and community. Talk to
your doctor and understand that antibiotics should not be used
for viral infections.
When
are antibiotics needed and when they are not needed?
These complicated questions are best answered by your doctor and
the answer depends upon the specific diagnosis. Here are few examples:
Ear infections: There are several types. Most need antibiotics,
but some do not.
Sinus infections: Most children with thick or green mucous do
not have sinus infections. Antibiotics are needed for some long-lasting
or severe cases.
Cough: Children do not need antibiotics for cough.
Fever: Antibiotics are not for fever but for bacterial infections.
Sore throat: Most cases are caused by viruses. Only one main type,
“ strep throat”, requires antibiotics. This kind must
be diagnosed by lab test.
Colds: Colds are caused by viruses and may sometimes last for
2 weeks or more. Antibiotics should never be used for cold. Same
home care remedy as hot lemon water, warm honey water often soothes
the throat.
Are
over the counter cough mixtures are helpful?
Over the counter cough mixtures are not helpful in children. More
over these preparation contains medicines which make the child
drowsy, irritable with dry mouth and throat. This will cause more
deterioration in his illness. A child on cough mixtures will cough
more and the duration of cough prolongs.
The
infection may change
Viral infections may sometimes lead to bacterial infections. But
treating viral infections with antibiotics to prevent bacterial
infections does not work, and may lead to infection with resistant
bacteria. Keep your doctor informed if the illness gets worse
or lasts a long time, so that proper treatment can be given, as
needed.
The
signs if you see, you must take your child to a doctor:
Lethargy, convulsion, vomits every thing, does not swallow, very
high fever, rash, breathing fast, acute onset of noisy breathing,
not passing urine for more than 12 hours or if you are worried.
|
|
As
a parent you are in best position to note your child's development
and milestones given below can be used as guidelines. No two children
develop at same rate, every child develops at his own pace. You
can talk about this to your Paediatrician in your next visit
|
6
WEEKS
Gross Motor
When child is pulled to sit, his head lags considerably but not
completely.
Your child intermittently raise his chin off the couch in prone
position.
Hands
The child keep his/her hands open most of the time.
Vision
Your child fix eyes on objects and follows a moving person up to
90 degrees?
General understanding
Your child smile at the mother in response to overtures.
|
12
WEEKS
Gross
Motor
If your child is held upright is he able to support his head for
few minutes.
Your child can hold chin and shoulders off couch and weight is borne
on forearm in prone position. |
 |
Hands
Your child keep hands frequently loosely open?
Vision
Your child follow-dangling toy from side to side (180
degrees)?
Your
child promptly looks at object in midline.
Hearing
Your child turn head to sound.
Vocalization
Your child respond when spoken to and makes squeaks of pleasure.
20 WEEKS
Gross
Motor
Your child put his/her weight on forearms when lying in prone
position.
Your child put his feet to mouth in supine position?
When child is pulled to sit, there is no head leg.
Hands
Your child able to grasp object voluntarily?
General understanding
Your child smile at his/her mirror image?
|
| 28
WEEKS Gross
Motor
Your
child sit with hands on couch for support.
Your child roll from supine to prone.
Hands
Your child feeds self with biscuit.
Cubes
Your child transfer cube from hand to hand?
General understanding
Your child imitate simple acts.
Your child respond to name(s). |
 |
Speech
Your
child speak syllabels like da,ba,ka
36
WEEKS
Gross
Motor
Your child sits without support for few minutes.
Your baby crawls
Hands
Your child picks up objects of size of currant between tip of
finger and thumb.
Cubes
Your child compares two cubes by bringing them together.
|
| 44
WEEKS Your
child will creep with abdomen off couch.
Your child will put object in and out of container.
Your child will say one word with meaning.
Dressing
Your child will hold arms out for sleeve or feet out for shoe.
|
 |
1
Year
Gross
Motor
Your child walks one hand held.
Your child says two or three words with meaning.
Your child walks on hands and feet like a bear when prone.
Your child understands the meaning of where is book? where is
shoe?
|
18
Months
Your
child walks upstairs one hand held.
Your child makes tower of three cubes.
Your child takes off his shoes by himself.
Your child feeds himself without much spilling.
2½ Years
|
 |
Your child jumps with both feet.
Your child knows full names.
Your child knows whether he is a boy or girl?
Your child helps to put things away.
Your child names at least one colour.
Your child makes a tower of eight cubes.
4 Years Your
child goes downstairs, one foot per step.
Your child can button clothes fully.
Your child names pictures in books.
Your child can tell you what action is taking place in a picture.
Your child uses action words(Verbs).
Your child copies cross.
Your child plays imaginative plays with doll.
5
Years
Your
child skips on both feet.
Your child can tie shoelaces.
Your child can copy a triangle.
Your child can name four colours.
Your child can react well when you leave him with a friend or
baby sitter.
Your child can name a coin correctly.
|
 The
first three years of life are a time of amazing learning for young
children and for the people who care for them every day. In these
years, most children develop new skills in a predictable order
they crawl before they walk and they point before they use words
to tell you what they want.
But every child is unique.
Every child develops at his own pace and reacts to people and
the world in his own way.
Every child has his own style of communicating with you.
It is important to remember that every child develops in his own
style and at his own pace. However, if you are concerned about
your child's development and would like to request an evaluation
(developmental assessment), please contact Prof. Pushpa Raj Sharma
for special appointment.
|
|
Chicken pox
Chickenpox
is a highly contagious illness by the varicella zoster virus and
occurs most commonly in late winter or early spring. Chickenpox
is spread by both direct contact with an infected person and through
air borne spread of respiratory secretions. Since infected persons
are contagious for 1-2 days before they even develop a rash, your
child may have been exposed to someone with chickenpox without knowing.
You can also get chickenpox after having direct contact with someone
who has shingles or herpes zoster, a reactivation of chickenpox.
Symptoms begin with a low grade fever, loss of appetite and decreased
activity. About two days later, your child will develop an itchy
rash consisting of small red bumps that start on the scalp, face
and trunk and then spread to the arms and legs (but may also occur
in the mouth and genitalia). The bumps then become blisters with
clear and then cloudy fluid, and then become open sores and finally
crust over within about twenty four hours, but your child will continue
to get new bumps for about four more days.
All of the chickenpox lesions should be crusted over after about
six days at which time your child will no longer be contagious.
It may take another one to two weeks before all of the scabs finally
heal. Once your child has had chickenpox he should have lifelong
immunity.
There is no effective treatment for children who develop uncomplicated
chickenpox, but if your child is given the Varivax vaccine within
72 hours (and sometimes up to five days) of being exposed to someone
with chickenpox, it may help prevent him from becoming infected.
The usual treatments are aimed at making your child more comfortable,
and can include pain relievers, plenty of fluids, oatmeal baths,
calamine lotion, and oral Benadryl for severe itchiness. Also keep
your child's fingernails cut short and allow him to wear loose fitting
clothing.
Treatment with acyclovir, an antiviral medication that can help
to decrease the symptoms of chickenpox, should be considered for
children at risk of developing a severe case of chickenpox. This
includes children with pulmonary
disorders, on steroid medications, or with immune system problems.
Croup
Croup, also called laryngotracheobronchitis, most commonly affects
children between the ages of six months and three years, usually
during the late fall, winter and early spring. Symptoms, which often
include a runny nose and a brassy cough, develop about 2-6 days
after being exposed to someone with croup.
One of the distinctive characteristics of croup is the abrupt or
sudden onset of symptoms. Children will usually be well when they
went to bed, and will then wake up in the middle of the night with
a croupy cough and trouble breathing. The cough that children with
croup have is also distinctive. Unlike other viral respiratory illnesses,
which can cause a dry, wet, or deep cough, croup causes a cough
that sounds like a barking seal.
Another common sound or symptom of croup is inspiratory stridor,
which is a loud, high-pitched, harsh noise that children with croup
often have when they are breathing in. Stridor is often confused
with wheezing, but unlike wheezing, which is usually caused by inflammation
in the lungs, stridor is caused by inflammation in the larger airways.
The pattern of symptoms in children with croup is also characteristic.
In addition to beginning in the middle of the night, symptoms, which
are often better during the day, worsen at night, although they
are usually less intense each night. Symptoms also become worse
if your child becomes anxious or agitated.
The symptoms of croup are caused by inflammation, swelling and the
buildup of mucus in the larynx, trachea (windpipe) and bronchial
tubes. Since younger infants and children have smaller airways,
it makes sense that they are the ones most affected by croup. In
contrast, older children will often just develop cold symptoms when
they are infected by the same virus.
Children with croup will usually also have a hoarse voice, decreased
appetite and a fever, which is usually low grade, but may rise up
to 104 degrees F.
Croup Assessment
Because of the characteristic signs and symptoms of croup, this
diagnosis is usually fairly easy to make. You can often tell a child
has croup while they are still in the waiting room or before you
enter the exam room, therefore, testing is usually not necessary.
Specifically, an xray is usually not required, and is usually only
done to rule out other disorders, such as ingestion of a foreign
body. When an xray is done, it will usually show a characteristic
'steeple sign,' which shows a narrowing of the trachea.
When assessing a child with croup, it is important to determine
if he is having trouble breathing. Fortunately, most children have
mild croup and have no trouble breathing, or they may only have
stridor when they are crying or agitated. Children with moderate
or severe croup will have rapid breathing and retractions, which
is a sign of increased work of breathing. They may also have stridor
when they are resting.
The croup score is an easy and standardized way to figure out if
a child has mild, moderate or severe croup, which can help to dictate
what treatments are necessary. The croup score is based on a child's
color, level of alertness, degree of stridor, air movement, and
degree of retractions, with 0 points given if these findings are
normal or not present, and up to 3 points given for more severe
symptoms.
Inspiratory Stridor |
- None
(0 points)
-
When agitated (1 points)
-
On/off at rest (2 points)
-
Continuous at rest (3 points)
|
| Retractions
|
-
None (0 points)
-
Mild (1 points)
-
Moderate (2 points)
-
Severe (3 points)
|
| Air
Movement/Entry |
-
Normal (0 points)
-
Decreased (1 points)
-
Moderately decreased (2 points)
-
Severely decreased (3 points)
|
| Cyanosis
(Color) |
-
None (0 points)
-
Dusky (1 point)
-
Cyanotic on room air (2 points)
-
Cyanotic with supplemental oxygen (3 points)
|
| Level
of Alertness (Mentation) |
-
Alert (0 points)
-
Restless or anxious (1 points)
-
Lethargic/Obtunded (2 points)
|
In
general, children with a croup score of less than 4 have mild croup,
5-6 have mild/moderate croup, 7-8 have moderate croup, and greater
than 9 have severe croup.
If you are unsure how severe your child's symptoms are, call your
Pediatrician.
Skin
infections or impetigo
Symptoms
Children with impetigo usually develop honey colored crusted lesions,
usually beginning in areas where the skin has been broken, irritated
or damaged. The nostrils, especially in kids with a runny nose,
are commonly affected. Untreated infections can quickly spread
to other areas on the child's body.
Bullous
impetigo cause much larger skin lesions that look like blisters
that quickly rupture and commonly affects a child's trunk or buttocks.
Diagnosis
Although cultures can be done, diagnosis is usually based on the
typical appearance of the rash.
Treatments
For small areas of infection, an over-the-counter or prescription
strength topical antibiotic may be all that is needed, in addition
to washing the area with warm soapy water. For more extensive
or persistent infections, an oral antibiotic might be needed.
What You Need To Know
|
- the
most common strains of bacteria that cause impetigo include
group A beta-hemolytic streptococci (GABHS) and Staphylococcus
aureus.
-
impetigo is spread by direct contact with infected lesions.
Children are usually no longer contagious once they have been
on antibiotics for 24-48 hours and there is no longer a discharge
or you are seeing signs of improvement.
-
folliculitis is a similar infection that involves hair follicles
-
glomerulonephritis, which can cause hematuria (bloody urine)
and high blood pressure, is a rare complication of having impetigo.
|
|
 |
|
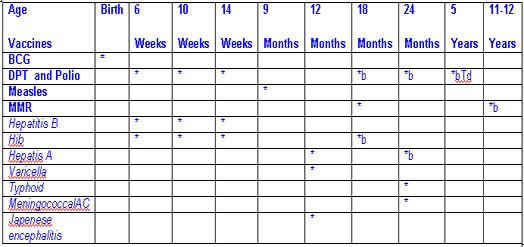
- Hepatitis
B vaccine (Hep B). If possible all infants should receive the
first dose of hepatitis B vaccine soon after birth or before
hospital discharge; The second dose should be given at least
4 weeks after the first dose. The third dose should be given
at least 6 months after the first dose.
However, the first dose can be given at 6 weeks along with DPT,
second dose at 10 weeks along with second dose of DPT and third
dose could be given at 9 months along with measles vaccination.
-
Tetanus and diphtheria toxoids (Td). It may be administered
at the age of 5 years.
-
Haemophilus influenzae type b (Hib) conjugate vaccine. If not
given as mentioned as in the schedule during first year, only
two doses are required at the interval of two months if given
after one year.
-
Measles, mumps, and rubella vaccine (MMR). The second dose of
MMR is recommended routinely at age 4-6 years but may be administered
during any visit, provided at least 4 weeks have elapsed since
the first dose and that both doses are administered beginning
at or after age 12 months. Those who have not previously received
the second dose should complete the schedule by the 11-12 year
old visit.
-
Typhoid Vaccine ( Vi antigen): First dose age 2 years and booster
doses at every 3 years.
-
Japanese Encephalitis Vaccine. This vaccine can be used for
children residing and frequently visiting endemic Tarai region.
It is given at one year or any time after one year on 0,7 and
30 days.
-
Meningococcal AC vaccine. The first dose is given at 2 years
and booster doses are given every three years
|
What
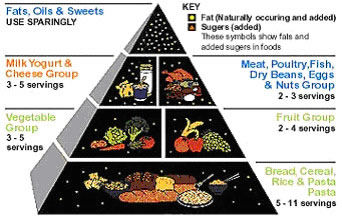
should be your child’s diet? |
The
following food pyramid shows the type of diet and frequency of meal.
Remember the child’s stomach is small and they can not take
large meal therefore give them small frequent meal. |
 |
Feeding
Recommendations During Sickness and Health
Up to 5 Months
of Age
Breastfeed as often as the child wants, day
and night, at least 8 times in 24 hours.
Do
not give other foods or fluids.
Breastfeed for at least 10 minutes each time
|
6 Months up to 12 Months Breastfeed
as often as the child wants.
Give
adequate servings of:
rice with dal, jaulo, halwa, roti with milk and sugar, khichadi,
lito, papaya, mango, banana
3
times per day if breastfed;
5 times per day if not breastfed.
12 Months up to
2 Years
Breastfeed
as often as the child wants.
Give
adequate servings of:
rice with dal, jaulo, halwa, roti with milk and sugar, khichadi,
lito, papaya, mango, banana
or family foods 5 times per day.
2 Years and Older
Give
family foods at 3 meals each day. Also, twice daily, give nutritious
food between meals, such as:
puffed rice with oil, roti, papaya, banana, mango, chiura, popcorn,
roast soya beans
What to do for diarrhoea?
1. GIVE EXTRA FLUID (as much as the child
will take)
Breastfeed
frequently and for longer at each feed.
If the child is exclusively breastfed, give ORS or clean water
in addition to breastmilk.
If the child is not exclusively breastfed, give one or more of
the following: ORS solution, food-based fluids (such as soup,
rice water, and yoghurt drinks), or clean water.
It
is especially important to give ORS at home when:
the child has been treated with Plan B or Plan C during this visit.
the child cannot return to a clinic if the diarrhoea gets worse.
MIX
AND GIVE ORS.
Up to 2 years 50 to 100 ml after each loose stool
2 years or more 100 to 200 ml after each loose stool
Give
frequent small sips from a cup.
If the child vomits, wait 10 minutes. Then continue, but more
slowly.
Continue giving extra fluid until the diarrhoea stops.
2. CONTINUE FEEDING
3.
Take your child to the health worker if:
lethargic, or convulsion occurs, or does not take orally,or blood
in the stool or vomits evry thing or develops high fever or does
not passes urine for 4 hours.
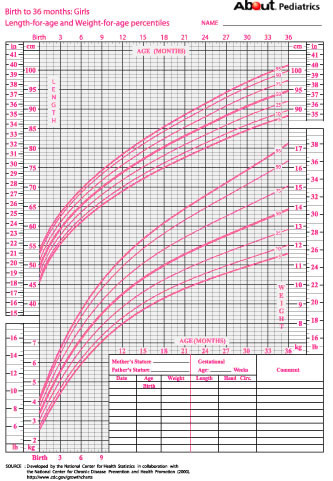
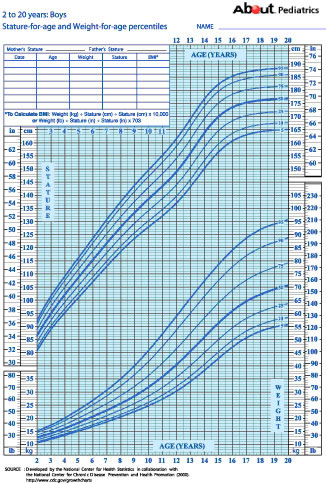
Find
out your childs growth using growth charts.
How to use these growth charts?
Growth charts are an important way to monitor your child's growth.
This guide will provide you with all of the information you need
to use and interpret the growth charts to follow how well your
child is growing. Find the age of your child and plot it on these
growth charts. If they are following a curve or parallel to that
curve then it indicates they are growing. They should never grow
below the third percentile. If they fall bellow the third percentile
of suddenly fall from their growing line consult your doctor.
Growth chart index
View all of the growth charts for infants and older children to
plot their height, weight and follow how well they are growing.
Boys: Birth to two years
Growth chart for boys from birth to age three years, with height
and weight growth curves combined on one easy to use colorized
sheet.
Girls: Birth to three years
Growth chart for girls from birth to age three years, with height
and weight growth curves combined on one easy to use colorized
(pink) sheet.
Boys two to twenty years
Growth chart for boys from two to twenty years, with height and
weight growth curves combined on one easy to use colorized (blue)
sheet.
Girls: two to twenty years
Growth
chart for girls from two to twenty years, with height and weight
growth curves combined on one easy to use colorized (pink) sheet.
|
 |
 |
 |
When should you start LITO to your
child? How you should feed LITO to your baby?
Never start solid food before completing 6 months of age. This
is because they can not swallow solid at this age and if you make
it thin so that your child can drink the calorie content will
be too low. When you feed thin “LITO” you child will
loose weight, urinate more frequently and will be constipated.
You should start solid only when your baby can swallow, can sit
with support, hold head erect and turn round. The best way to
tell the right period for the solid food is when your child seems
to be asking for it. He is not likely to say, "Mom can I
please have solid foods?" It is more likely that when you
are eating he will look at you as if to say, "How come you
aren't giving me some of what you are having?" This communication
will likely be in the form of fussiness when you are eating. This
is a good time to begin solid foods, or you can begin anytime
you want using the guidelines stated above.
I recommend starting with rice cereal. Cereal should never be
given in bottle. Rice cereal can be prepared at home by cooking
rice and pureeing it in a blender or making a pate using cup and
spoon. As your child is taking milk by sucking, and it is the
first time child is on a thick feed s/he will try to push it by
protruding tongue. Therefore your baby's first rice cereal meal
should be thin. Once baby can swallow the feed you must go on
increasing its thickness. The cereal you have prepared must not
fall if you keep it in your finger. When your child is able to
swallow this thick cereal then only you should go on increasing
the amount of solid feed. Usually the amount of feed should be
equal to the number of teaspoon with the age of your child in
month (it is the uncooked powder not the cooked meal).
It is not necessary to buy the costly cereals available in the
market. Your child will need nearly two weeks to learn to swallow
the solid. You can use rice that is prepared for the family meal.
For first few days only small amount is needed. With the rice
cereal, place your baby in a propped up position, and move the
spoon towards his mouth. The first few days he will tend to push
the cereal right back out with his tongue. This is because babies
have a thrust reflex causing their tongue to thrust back out anything
that is put in their mouths. Within several days your baby will
begin to get the idea of closing his lips around the spoon and
swallowing. Once he does, you can begin to monitor the amount
of food he needs. In order to determine this, (which is not a
pre-determined amount, but varies from child to child) keep moving
the spoon towards his mouth and look for signs that he is losing
interest. If he turns his head away, clamps his lips shut, or
appears bored, it is time to stop. Otherwise, keep moving the
spoon to his mouth as long as he keeps opening it and looking
happy.
It is better to continue breast feeding even after you start solid.
Formula deeding is never necessary if you have breast milk. It
is not necessary to give water after each solid feed. You may
feed breast milk after the solid. After your baby has done well
with rice cereal, you can begin feeding him DAL or other meal.
Other solids can be introduced once he has been eating cereal
for a week or two and is tolerating it well (as long as he is
at least four months old). The next foods to be introduced --mostly
peas, green beans, squash, sweet potatoes, potatoes, and carrots.
Give your baby only one new food at a time. Be sure to wait three
to five days before starting another one to determine if he has
any reaction to a food, such as a rash, stomach pain, vomiting,
or diarrhea.
Always try thick solid. After nine months give your child the
LITO in a separate plate while you are eating. Let him play with
this and keep himself in his/her mouth. Let him/her see and practice
eating him/her self.
|
|
|